The spread of COVID-19 in spring 2020 consumed the United States’ healthcare system, shelving seemingly less-pressing medical concerns. Hospitals, clinics and patients alike postponed elective procedures and routine appointments.
But even sensible precautions have knock-on effects: Delayed or missed care can mean diseases go undetected and untreated.
With that in mind, a group of researchers led by Oguzhan Alagoz of the University of Wisconsin-Madison have analyzed the impact of COVID-enforced disruptions to preventative care on long-term breast cancer mortality.
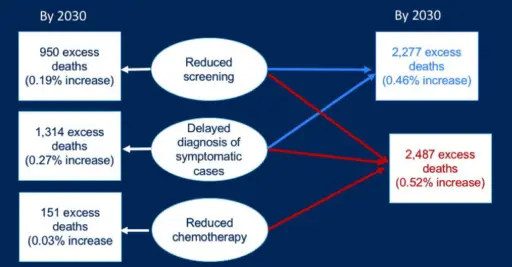
The researchers, who published their findings in a new paper in the Journal of the National Cancer Institute, discovered the effect was, thankfully, small. Their collaborative modeling study estimates that by 2030, 2,487 additional breast cancer deaths will occur due to the pandemic’s interruption of mammography screenings, symptomatic diagnoses and chemotherapy treatments. In all, that amounts to slightly greater than a half-percent (0.52%) increase over typical projections had the pandemic not transpired, which Alagoz says is a credit to healthcare providers’ ability to rebound and resume offering regular care within a few months.
“People were expecting like 10,000 or 15,000 additional deaths,” says Alagoz, the Proctor and Gamble-Bascom Professor of industrial and systems engineering. “Although at first the screening volumes and diagnostic procedures were delayed significantly, screening facilities and clinics were pretty good in catching up and they went back to normal very quickly. That’s the primary reason the mortality impact is actually limited.”
The study grew out of a preliminary analysis Alagoz and collaborators had conducted in late spring 2020 to inform a Science commentary by National Cancer Institute (NCI) Director Norman Sharpless. Alagoz also took part in an NCI-sponsored webinar on the pandemic’s impact on cancer data in October 2020.
To look deeper into the issue, Alagoz and his coauthors, including Amy Trentham-Dietz, a professor of population health sciences at UW-Madison, used data from the Epic Health Research Network and two Breast Cancer Surveillance Consortium registries to determine the volume of mammography screenings and diagnostic imaging from March to September 2020. They relied on expert opinions of oncologists to gauge the pandemic’s effect on treatment regimens.
Then, the researchers ran three independent mathematical models, including the Wisconsin-Harvard Breast Cancer Epidemiology Simulation Model that Alagoz and Trentham manage along with Natasha Stout, a UW-Madison graduate who’s now an associate professor at Harvard. The model is one of six that make up the NCI-funded Cancer Intervention and Surveillance Modeling Network.
While the overall results were encouraging, Alagoz notes that any additional deaths are still premature losses of life. And, given that the models revealed reductions in mammography screenings and diagnostic visits were the overwhelming drivers of increased deaths, he says it’s important that both patients and healthcare providers work to ensure women who missed their regularly scheduled mammograms make them up, rather than waiting until their next planned screenings.
He says this kind of analysis can help healthcare providers and policymakers set priorities when responding to future scenarios, be it a pandemic that halts routine care or another crisis that exhausts resources.
“This is focused on breast cancer, but to me, this situation affects all diseases,” he says. “This is beyond breast cancer.”
This work was supported by the National Institutes of Health under National Cancer Institute Grants U01CA152958, U01CA253911 and R01CA248068. Supported in part by National Cancer Institute at the National Institutes of Health grant R35CA197289. Collection of Breast Cancer Surveillance Consortium data used in this study was supported by National Cancer Institute Grants P01CA154292, U54CA163303, grant R01 HS018366-01A1 from the Agency for Healthcare Research and Quality, and award PCS-1504-30370 from the Patient-Centered Outcomes Research Institute.