With a thin probe and a burst of microwaves, doctors can eradicate cancer cells without opening up a patient for surgery.
But when you’re trying to cook a tiny amount of precancerous tissue to death in an area as delicate as, say, the esophagus—where muscles control the flow of food into the stomach—precision is paramount.
A team of University of Wisconsin-Madison biomedical engineers is working to hone new imaging techniques that could allow for finer monitoring of this kind of minimally invasive ablation treatment.
In an exploratory study recently published in the journal Biomedical Optics Express, College of Engineering graduate students Ryan Niemeier, Sevde Etoz and Daniel Gil and faculty members Jeremy Rogers, Melissa Skala and Christopher Brace analyzed how two different methods of optical coherence tomography (OCT) could provide valuable, quantitative imaging data on tissue that’s been ablated and the surrounding areas.
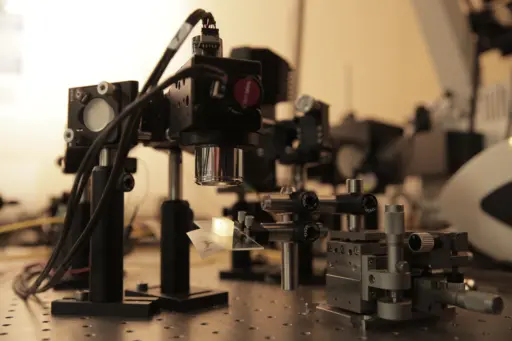 This custom-built optical coherence tomography instrument uses visible light to view tissue.
This custom-built optical coherence tomography instrument uses visible light to view tissue.
Unlike ablations of tumors in organs such as the liver or lung, where the measurements are in centimeters, procedures in areas like the esophagus work in scales of fractions of a millimeter.
“Traditional medical imaging doesn’t really work well for that,” says Brace, an associate professor of biomedical engineering who led the ablation side of the study. “Traditional optical visualization might give you a sense of what’s happened on the surface, but you can’t quite tell how deep it got.”
To explore an alternative method, the UW-Madison engineers used a traditional weakness of optical technology to their advantage. When light is beamed into tissue, it scatters, limiting the depth and contrast of the resulting image.
“At the same time, it’s also an opportunity,” says Rogers, an assistant professor of biomedical engineering whose lab focuses on biomedical optics. “Scattered light actually contains a lot of information. So by making use of that scattering signal, we can actually turn that into a source of contrast.”
OCT, which Rogers likens to the optical version of ultrasound, typically uses near-infrared light, which scatters less and penetrates deeper than visible light. But since the group was expressly interested in examining changes in scattering, the visible wavelength offered intriguing potential.
Rogers and his optics team custom built an OCT instrument that uses visible light and then compared the images to those taken with a commercially developed system employing near-infrared light.
“What we’ve seen with this is that they actually contain complementary information. Each has certain advantages and disadvantages,” says Rogers, noting the near-infrared tool sees deeper and has a better signal-to-noise ratio, while the visible instrument yields a higher resolution.
“We also know from theory of scattering that these different wavelength ranges are going to actually be sensitive to different structures in the tissue.”
Thus, detecting changes in scattering could indicate physical tissue changes, such as cell death in the case of ablation treatments. With further exploration, that could mean real-time monitoring of procedures, which could increase efficiency—no more waiting on lab work to confirm results.
“It suggests we might be able to use this type of technique to look more interactively at what’s happening in the tissue,” says Brace.