As the COVID-19 pandemic continues to spread across the United States and the world, many are putting their hope in science to bring an end to the virus, or at least make it manageable. But it’s not just virologists and epidemiologists who will find the way forward. Researchers from all sorts of disciplines are pivoting their research to help out with the pandemic.
 John Yin
John Yin
One is John Yin, Vilas Distinguished Achievement Professor in the Department of Chemical and Biological Engineering at the University of Wisconsin-Madison, who uses experimental and computational methods to understand how viruses spread. Yin is working on several projects that could have a direct bearing on COVID-19, and says he’s ramping up work on them to help combat the virus.
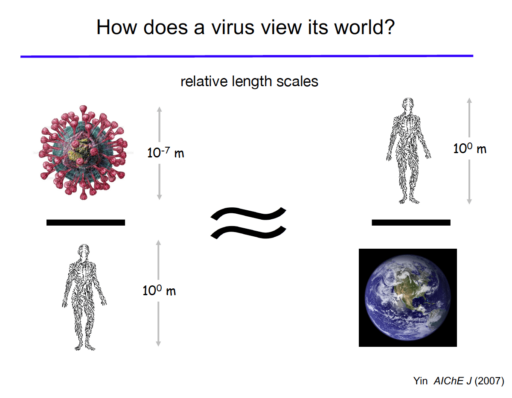
Yin says it may seem unusual for an engineer to specialize in viruses. But he says looking at these infectious particles through an engineering lens could be very useful. Chemical engineers often think about the ways that raw materials are processed to make products like fuels, plastics or pharmaceuticals. “What’s the connection to viruses? Well, when a virus enters the cell, it essentially turns the cell into a manufacturing process to make more virus,” he says. “Our engineering approaches try to take the molecular and cell biology that’s known and translate the verbal descriptions from biologists into a quantitative description by an engineer. Essentially, we end up writing equations to describe the various processes that are going on inside of this cell.”
Using that quantitative information, Yin uses powerful computers to model how viruses hijack cellular mechanisms to reproduce, how quickly they grow, how much “progeny” they produce, how they spread from cell to cell throughout the body, and even how people can transfer viruses to one another.
Currently, Yin is shifting some of his research to focus on the novel coronavirus. He says that one long-term project—studying beneficial defective interfering particles—could eventually be relevant to COVID-19.
Many viruses, including influenza, HIV and possibly COVID-19, are pretty sloppy when they replicate themselves. That’s because they carry RNA genomes that are inaccurately copied, leading to many more mutations and many “junk” particles that contain part of the virus genome but are incapable of reproducing. Many of these incomplete particles—the defective interfering particles—however, can still invade cells and hijack some of their resources, but they fail to make any products or cause illness.
But they’re not benign to fully-functioning viruses. “If they get into a cell with a virus, they can steal resources from it,” Yin says. “So, in essence, the junk particles are parasites of virus infections. And anything that’s bad for a virus infection is potentially good for the human hosts that are trying to stop the virus.”
Yin, who has worked on the particles with colleagues from the interdisciplinary Wisconsin Institute for Discovery, says he’s interested in developing models and experiments to show how defective interfering particles could be used as a therapeutic to control or manage viral infections. And because the defective interfering particles essentially co-evolve with the virus they are derived from, it’s unlikely the virus could mutate or develop an immunity to them like they can with drug therapies.
 Credit: John Yin
Credit: John Yin
While Yin isn’t focusing on how the therapy might work, he says people could take the defective interfering particles to stimulate their immune system, ramp up defense signaling in cells, and hopefully ward off infection. It’s also possible that after infection, people could take defective interfering particles via a nasal spray or other delivery mechanism to reduce the severity of an infection. That, however, is very far off, and Yin says there is still much to understand about defective interfering particles before they ever end up at the pharmacy.
Right now, Yin says the best solutions to COVID-19 would be a vaccine and new antiviral drugs—and another of his projects is focused on making drug testing much faster.
The gold standard test for most antiviral drugs is via a technique called a plaque-assay. Researchers release a virus onto a dish of cells overlaid with a layer of semi-solid agar to force the virus to spread only to neighboring cells. Over time, as the viruses land and infect the fabric of cells, they make holes or plaques which are visible to the naked eye. The number of plaques that develop can tell researchers how effective a drug is at inhibiting or reducing the viral load.
Yin and his former graduate student Ying Zhu found that replacing the agar with a thin layer of a flowing liquid medium makes the assay 10 to 1,000 times more sensitive. It also speeds up the plaque-assay process from three to five days to just one or two days. It’s a method that could more easily be automated or used with digital imaging, meaning it could speed up assessment of dozens or even hundreds of potential antiviral drugs. Currently, Yin is hoping to commercialize the advance with the help of the Wisconsin Alumni Research Foundation.
Yin says that he and his team are also interested in bringing their computational expertise to bear on COVID-19. “We are in the early stages of developing a simulation of the growth of coronaviruses when they get into cells. That might have a use in helping to identify targets for antiviral drugs,” he says. “There’s a lot of literature about coronaviruses and we’re starting to look at some of that.”
Yin is hoping that his research, as well as that of hundreds of other researchers across disciplines, will soon get a little extra boost. The COVID-19 stimulus bill passed by the U.S. Congress during the last week of March 2020 added an extra $75 million to the National Science Foundation’s Rapid Response Research award program for projects that will help prevent, prepare for, and respond to the ongoing coronavirus pandemic. Yin has submitted several grant proposals and hopes his research can be part of a wave of science used to limit this and any future pandemics.