How a mechanical engineer hopes to influence the ubiquitous surgery’s success, one patient at a time
Deb Constien recalls a time years ago when climbing the stairs of her house to get to her young son’s room would trigger jolts of pain in her knee.
“In the year and a half that we lived in that house, I can count on both hands the number of times I was able to go upstairs to my son’s bedroom,” she says. “That’s how bad the pain in my knee was.”
Constien was diagnosed at 13 with rheumatoid arthritis, which causes inflammation in the joints. By age 29, the pain in her left knee had become so severe that she needed a total knee replacement.
The procedure was life-changing. It eliminated her knee pain, allowing her to do many activities again, including using stairs, gardening and going for walks. Now, some 20 years after the procedure, Constien’s artificial knee is holding up well—but there are a few nagging issues. Her knee implant sometimes makes annoying clicking sounds. And she is unable to kneel on that knee. “It doesn’t really feel like a normal knee, and it doesn’t function the same way, so I need to change how I do some activities,” says Constien, 54, who lives in Sun Prairie, Wisconsin.
Dr. Richard Illgen, a professor of orthopedic surgery in the University of Wisconsin School of Medicine and Public Health, says Constien’s experience after a knee replacement isn’t uncommon. “If you ask patients a year after the procedure if their knee feels normal, most of them will say no,” he says. “Even if patients are generally satisfied with their knee, it’s a far cry from a normal knee for most people.”
And some patients have much worse outcomes. Up to 20% of patients report not being satisfied with their total knee replacement—experiencing pain, stiffness or limited mobility, according to a 2010 study published in the journal Clinical Orthopaedics and Related Research.
That’s why our engineers are working on technologies that could unlock better outcomes for most total knee replacement patients.
Making it personal
For patients with osteoarthritis of the knee, which occurs when the cartilage that cushions the ends of bones wears down, a total knee replacement is the final treatment option for relieving the pain. It’s a major surgery in which orthopedic surgeons remove the damaged cartilage and bone from the joint and install implants made of metal and plastic to create an artificial knee joint. Approximately 790,000 total knee replacements are performed annually in the United States, making it one of the most common orthopedic procedures, according to the American College of Rheumatology.
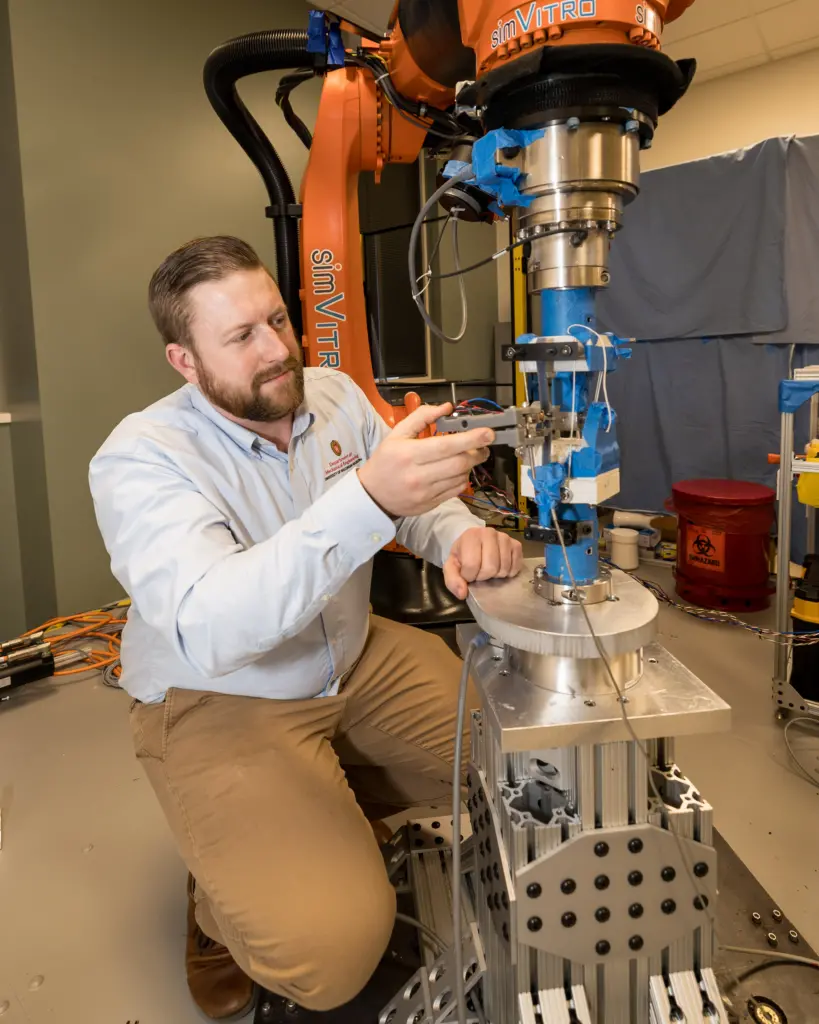 Assistant Professor Josh Roth places his ligament tension sensor on a ligament phantom attached to their surrogate knee joint to take validation measurements. In the future, such a sensor could enable surgeons to make crucial measurements during total knee replacement procedures. Credit: Joel Hallberg.
Assistant Professor Josh Roth places his ligament tension sensor on a ligament phantom attached to their surrogate knee joint to take validation measurements. In the future, such a sensor could enable surgeons to make crucial measurements during total knee replacement procedures. Credit: Joel Hallberg.
Traditionally, surgeons have prepared every patient’s artificial knee in the same way, aiming for a neutral mechanical alignment designed to maximize the longevity of the implant.
“However, there’s a lot of variability in human anatomy and in how people’s joints function,” Illgen says. “The next big step for improving outcomes for total knee replacement patients is moving from a general one-size-fits-all approach to more personalized surgical procedures that are tailored to a specific patient’s unique anatomy and joint biomechanics.”
But there’s a barrier to realizing this goal: We don’t currently have sufficient biomechanical data to effectively personalize these procedures.
That’s where Mechanical Engineering Assistant Professor Josh Roth’s research comes in. He’s working to enhance surgical planning for total knee replacements by characterizing how the joint and ligament biomechanics change as a patient’s osteoarthritis becomes more severe. To do this, Roth is developing sensors that will provide better measurements of these biomechanics in the patients themselves.
During a total knee replacement procedure, a surgeon needs to adjust the tension of the ligaments to achieve proper balance and stability in the knee. But that can be a tricky task, as surgeons don’t have a way to objectively measure the tension in an individual ligament. So Roth is developing a tool—a novel handheld sensor—that will enable surgeons to make these crucial measurements during the procedure. “Our sensor could be used as a quality-control check during surgery to allow surgeons to identify and correct individual structures that may be improperly tensioned—which should mitigate postoperative pain, stiffness and instability,” he says.
In the future, Roth envisions that clinicians could also use this sensor to measure a patient’s biomechanics before surgery. These measurements, along with previously collected biomechanical data and medical imaging of the patient’s anatomy, would help surgeons decide which implants to use and how to optimally align them on a particular patient’s bones.
In addition, Roth’s group is working on developing a medical imaging technique that uses ultrasound to view how a patient’s joint moves. This imaging technique, which doesn’t expose a patient to radiation, promises to provide more detailed information about how a joint behaves. “So, we can have a patient walk, or squat, or stand up from sitting in a chair to get a much better idea of how that patient’s joints are moving during daily living activities,” Roth says. “This information will enable more personalized surgical plans.”
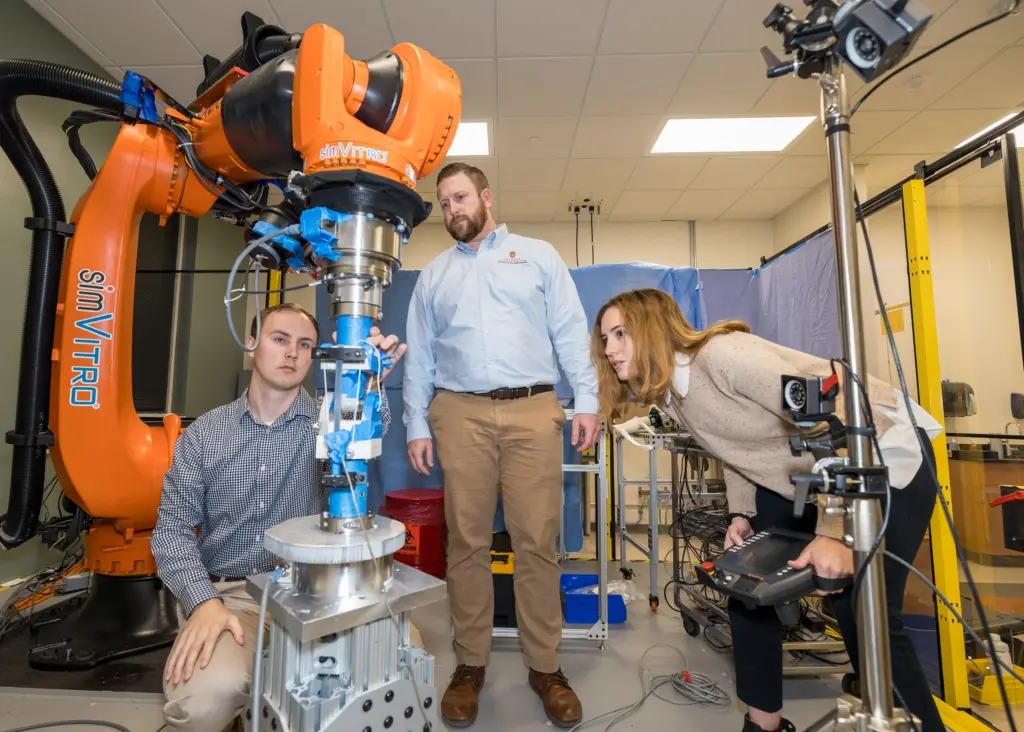 Biomedical engineering graduate students Matthew Blomquist and Lesley Arant and Mechanical Engineering Assistant Professor Josh Roth (center) set up a surrogate knee joint to conduct mechanical testing using a robotic arm in Roth’s lab. Credit: Joel Hallberg.
Biomedical engineering graduate students Matthew Blomquist and Lesley Arant and Mechanical Engineering Assistant Professor Josh Roth (center) set up a surrogate knee joint to conduct mechanical testing using a robotic arm in Roth’s lab. Credit: Joel Hallberg.
A helping robotic hand
In recent years, the orthopedics industry has introduced computer navigation and robotic assistance technologies that allow surgeons to perform total knee replacements with extraordinary precision. The use of these technologies is growing, with robotic assistance now being used in more than 13% of total knee replacements, according to the 2023 annual report of the American Joint Replacement Registry on hip and knee arthroplasty.
Roth is excited by the possibilities of pairing the tools he’s developing with the capabilities of cutting-edge surgical robots.
“The technologies we’re developing in my lab will enable us to discover subtle tweaks that can be made to total knee replacements that improve patient outcomes,” Roth says. “And now robots are allowing surgeons to precisely execute small tweaks in the procedure that they couldn’t do before. By harnessing these technologies, we have a great opportunity to significantly improve patients’ satisfaction with their artificial knee.”