A new, low-cost wound dressing developed by University of Wisconsin-Madison engineers could dramatically speed up healing in a surprising way.
The method leverages the energy generated from a patient’s own natural body motions to apply gentle electrical pulses at the site of an injury.
In rodent tests, the dressings slashed healing times from roughly two weeks (for untreated injuries) to a mere three days.
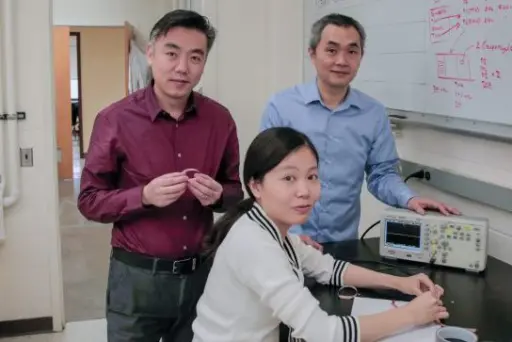 Professor Xudong Wang, left, holds a prototype wound-healing device that generates energy from body movements. Graduate student Yin Long, seated, and visiting radiology professor Hao Wei collaborated on development of the new device. Photo credit: Sam Million-Weaver.
Professor Xudong Wang, left, holds a prototype wound-healing device that generates energy from body movements. Graduate student Yin Long, seated, and visiting radiology professor Hao Wei collaborated on development of the new device. Photo credit: Sam Million-Weaver.
“We were surprised to see such a fast recovery rate,” says Xudong Wang, a professor of materials science and engineering at UW-Madison. “We suspected that the devices would produce some effect, but the magnitude was much more than we expected.”
Wang and collaborators described their wound dressing method Nov. 29, 2018, in the journal ACS Nano, which also highlighted the paper as an editor’s choice.
Researchers have known for several decades that electricity can be beneficial for skin healing, but most electrotherapy units in use today require bulky electrical equipment and complicated wiring to deliver powerful jolts of electricity.
“Acute and chronic wounds represent a substantial burden in healthcare worldwide,” says collaborator Angela Gibson, an assistant professor in the Department of Surgery at UW-Madison. “The use of electrical stimulation in wound healing is uncommon.”
In contrast with existing methods, the new dressing is much more straightforward.
“Our device is as convenient as a bandage you put on your skin,” says Wang.
The new dressings consist of small electrodes for the injury site that are linked to a band holding energy-harvesting units called nanogenerators, which are looped around a wearer’s torso. The natural expansion and contraction of the wearer’s ribcage during breathing powers the nanogenerators, which deliver low-intensity electric pulses.
“The nature of these electrical pulses is similar to the way the body generates an internal electric field,” says Wang.
And, those low-power pulses won’t harm healthy tissue like traditional, high-power electrotherapy devices might.
In fact, the researchers showed that exposing cells to high-energy electrical pulses caused them to produce almost five times more reactive oxygen species—major risk factors for cancer and cellular aging—than did cells that were exposed to the nanogenerators.
Also a boon to healing: They determined that the low-power pulses boosted viability for a type of skin cell called fibroblasts, and exposure to the nanogenerator’s pulses encouraged fibroblasts to line up (a crucial step in wound healing) and produce more growth factors.
“These findings are very exciting,” says collaborator Weibo Cai, a professor of radiology at UW-Madison. “The detailed mechanisms will still need to be elucidated in future work.”
In that vein, the researchers aim to tease out precisely how the gentle pulses aid in healing. The scientists also plan to test the devices on pig skin, which closely mimics human tissue.
And, they are working to give the nanogenerators additional capabilities—tweaking their structure to allow for energy harvesting from small imperceptible twitches in the skin or the thrumming pulse of a heartbeat.
Gibson is optimistic about the team’s results. “The impressive results in this study represent an exciting new spin on electrical stimulation for many different wound types, given the simplicity of the design,” she says. Gibson will collaborate with the team to confirm the reproducibility of these results in human skin models.
If the team is successful, the devices could help solve a major challenge for modern medicine. “We think our nanogenerator could be the most effective electrical stimulation approach for many therapeutic purposes,” says Wang.
And because the nanogenerators consist of relatively common materials, price won’t be an issue: “I don’t think the cost will be much more than a regular bandage,” says Wang. “The device in itself is very simple and convenient to fabricate.”
Weibo Cai is the Vilas Distinguished Achievement Professor in the Department of Radiology at UW-Madison. Angela Gibson is a burn surgeon and director of wound healing services at UW Health. The research was supported by the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health under award numbers R01EB021336 and P30CA014520.